THE (ROBOT) DOCTOR WILL SEE YOU NOW
With the NHS in crisis, and waiting times on the rise, hospitals and doctors are turning to new technologies for diagnosis, treatment and prevention of diseases and chronic conditions. These technologies, whether recently launched or still in development, aim to improve patient outcomes and relieve the burden on healthcare professionals and providers. From minimally invasive treatments for cancer to toilet seats that measure vital signs, and bras that detect breast cancer to implantable soft robotics that deliver tailored drugs, these innovations have the potential to revolutionise healthcare of the future.
We put the spotlight on 10 engineering innovations designed to improve healthcare experiences for patients and doctors
1
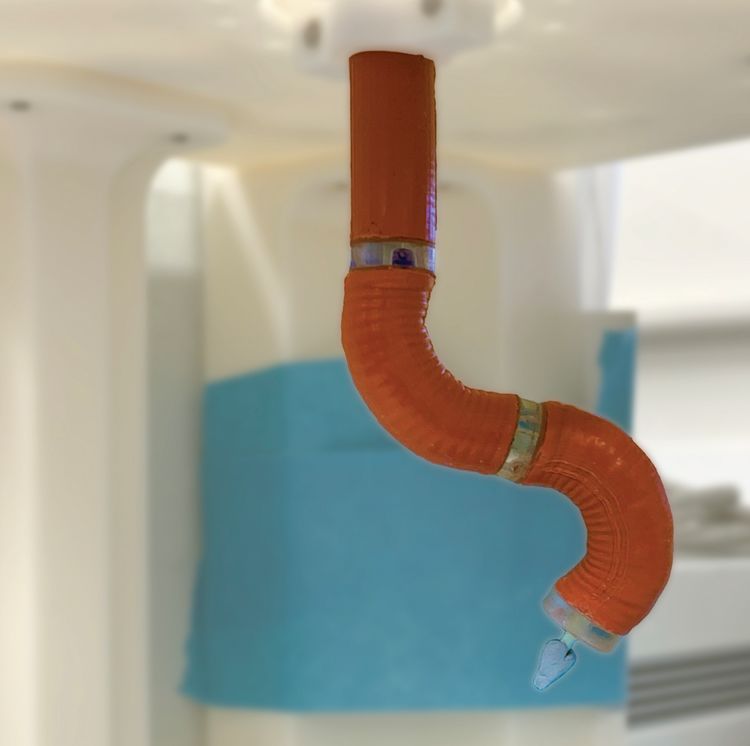
Soft robotics in bowel cancer surgery
Bowel cancer, also known as colorectal cancer, is treated using a combination of different treatments, with surgery being the main and most effective.
“There is a trend towards treatments using minimally invasive approaches, since these reduce risk for the patient and cost. However, the existing tools for procedures to cut and remove tumours are limited to manual endoscopes, which suffer from limited dexterity,” says Ferdinando Rodriguez y Baena, professor of medical robotics in the Department of Mechanical Engineering at Imperial College London.
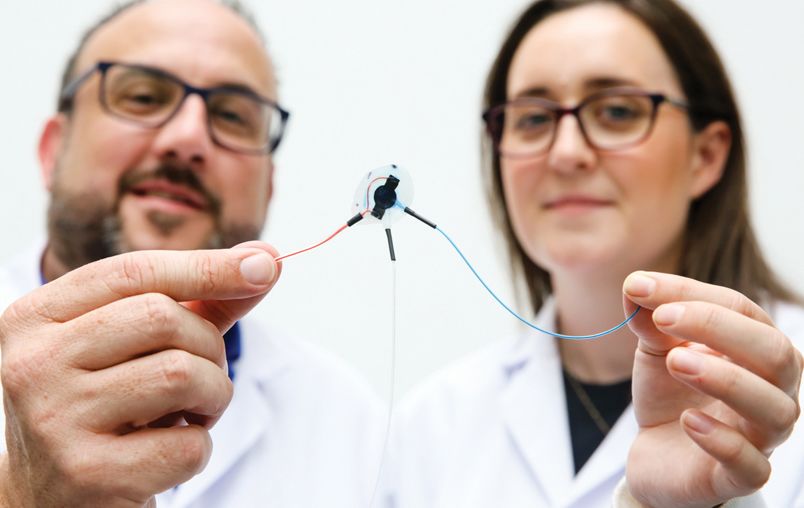
Having conducted research into soft robots for minimally-invasive surgery for a number of years, the Imperial team has developed a soft robotic manipulator intended for use in colorectal surgery.
Baena says: “By offering the option of performing surgery endoluminally with dexterity and precision that would rival open surgeries, the system we are proposing has the potential to improve care and reduce risks.
“The robot is unique since it uses pressure for actuation and has a morphing design, where its silicone structure deforms internally to maximise force when pressurised. We believe that the use of pressure for actuation, rather than the more traditional tendons, can enable surgeries deep in the colon, without being affected by bends in the transmission lines.”
Having produced one robot arm to demonstrate the effectiveness of the actuation concept, a bi-manual version is now under way where one arm can carry a surgical scalpel and the other a gripper.
2
Wearable breast cancer monitor
Breast cancer patients have an almost 100% survival rate if the disease is detected early. However, if it goes unnoticed until the later stages, the survival rate drops to around 25%.
Massachusetts Institute of Technology researchers have created a wearable ultrasound device that can detect breast cancer early by taking regular images of the breast tissue.
With the use of a piezoelectric material, the research team was able to miniaturise the ultrasound scanner. The scanner is then housed in a flexible, 3D-printed patch that features honeycomb-like openings to ensure contact with the skin. The miniature scanner can be moved to six positions and can also rotate to ensure that the entire breast is scanned.
Attached to a bra using magnets, the patch can be used over and over again by those who are at high risk of breast cancer and by those who don’t have regular access to screening.
“This work will significantly advance ultrasound research and medical device designs, leveraging advances in materials, low-power circuits, AI algorithms and biomedical systems,” says Professor Anantha Chandrakasan, dean of MIT’s School of Engineering.


3
Smart toilet seat monitors vital signs
Patients suffering with chronic conditions often require regular monitoring by healthcare professionals. However, outside a healthcare setting this becomes challenging.
US-based Casana has developed a product that enables consistent and accurate at-home health monitoring throughout the day. Known as the Heart Seat, this smart toilet seat is embedded with sensors to measure a patient’s vital signs.
Austin McChord, CEO of Casana, says: “The key component of this technology is that it’s truly effortless – it doesn’t take any additional time out of your day.”
With the Heart Seat having been cleared by the US Food and Drug Administration for measuring heart rate and oxygen saturation, Casana is now working with researchers to also integrate blood pressure measurements into the seat.
Data from the battery-powered seat is transmitted via wi-fi to the Casana Cloud. This data and resulting insights can easily be viewed through a clinician interface.
“The seat could save valuable time for both providers and patients, potentially replacing doctors’ visits and hopefully some day hospital readmissions. By unobtrusively collecting key vital signs, you might even forget it’s there. It’s technology like this that truly makes our lives better,” says McChord.
4
Air quality monitor detects viruses
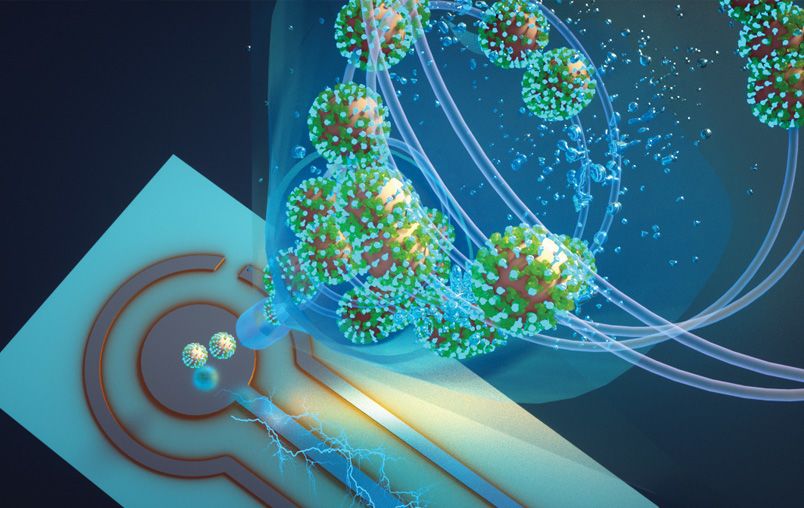
The Covid pandemic made us more aware of how easy it is to catch airborne viruses in crowded indoor areas. Researchers at Washington University in St Louis have developed a proof-of-concept air quality monitor that can detect whether Covid particles are in the air.
John Cirrito, professor of neurology in the university’s School of Medicine, says: “There is nothing at the moment that tells us how safe a room is. If you are in a room with 100 people, you don’t want to find out five days later whether you could be sick or not. The idea with this device is that you can know in real time, or every five minutes, if there is a live virus in the air.”
The research team adapted a biosensor originally developed to detect amyloid beta as a biomarker for Alzheimer’s disease to detect the spike protein for the SARS-COV-2 virus.
The biosensor is integrated into an air sampler that uses wet cyclone technology. Virus aerosols are trapped in fluid on the walls of the sampler that then sends it to the biosensor using electrochemistry.
Rajan Chakrabarty, associate professor in the McKelvey School of Engineering at the university, says: “The high virus recovery by the wet cyclone can be attributed to its extremely high flow rate, which allows it to sample a larger volume of air over a five-minute sample collection compared with commercially available samplers.”
The research team is now working to commercialise the monitor as well as looking at its potential use in detecting other airborne viruses, such as flu and rhinovirus.
5
Smart hearing health

With GP surgeries under increasing pressure, a new portable device is helping democratise ear and hearing healthcare by offering diagnosis and treatment in community-based settings.
This smartphone-enabled otoscope from Tympa Health offers an accessible solution to patients. For instance, pharmacies and care homes can now perform examinations, wax removal using a suction unit and a hearing check in less than 30 minutes.
Tympa partnered with Cambridge-based Team Consulting to develop the device. Oliver Sowerby, head of surgical technologies at Team Consulting, explains:
“There were three areas we needed to develop which were key to the device’s technical success: the optical magnification of the image; the illumination of the inner ear; and powering and charging the device.”
His colleague, Jon Jamin, senior engineering consultant, says: “The optical system was specified by a physicist and tested with larger off-the-shelf lenses. Once we knew the optical theory would work, the next step was miniaturising the system to fit to the back of an iPhone. An adjustable functional rig proved the image clarity was possible using components of the necessary size, in achievable manufacturing tolerances and within the form of a phone attachment.”
6
Tentacle robot in lung cancer surgery
Lung cancer diagnosis and surgery is an invasive procedure that can often require significant removal of tissue.
A team of engineers, scientists and clinicians at the University of Leeds STORM Lab is developing a far less invasive treatment with the use of a tiny, tentacle-like robot that can travel deep into the lung’s smallest bronchial tubes to detect and treat the first signs of cancer.
Measuring 2mm in diameter and controlled by magnetics, this ultra-soft surgical robot is able to shape itself to the anatomy and reduce trauma. The result is a device that is not only more accurate but also causes less tissue damage than standard equipment.
Professor Pietro Valdastri, director of the STORM Lab, says: “This new magnetic technology can allow us to reach way deeper into the human body than ever before in a way that doesn’t require extremely qualified surgeons, thanks to robotic guidance. We hope this will democratise cancer treatment and increase access to top-quality procedures.”
Having tested the magnetic tentacle robot on the lungs of a cadaver, the team is now collecting data to enable the start of human trials. Valdastri adds: “The same approach can be used to reach the deep part of the brain, pancreas, bladder and any other body cavity that is accessible through a narrow lumen. The cardiovascular system is also another potential district of use.”
Enjoying this digital edition of Professional Engineering? Please email profeng@thinkpublishing.co.uk with your thoughts and feedback to help us improve


7
Snake-like robot in throat cancer surgery
A thin snake-like robot developed for remote inspection in industrial applications has been adapted for use in throat cancer surgery.
At 5m long and 8.5m diameter and with six degrees of freedom, the Cobra is able to slither into small spaces and manoeuvre around tight bends. Devices such as cameras and lasers can be threaded through the interior to the ‘head’ of the robot to enable it to perform various requirements depending on the application.
“We started our research 10 years ago when Rolls-Royce approached us to develop a robot to navigate inside aero engines to perform remote repair and inspection. Having reached technology readiness level six, the robot has become an important monitoring tool in safety-critical applications,” says Abdelkhalick Mohammad, associate professor in mechatronics at the University of Nottingham, who is part of the Cobra research team.
Two years ago Dr Oladejo Olaleye, a consultant ear, nose and throat surgeon at University Hospitals of Leicester NHS Trust, asked the researchers to adapt the robot for use in the diagnosis and treatment of throat cancer. “This is an exciting overlap between robotic engineering and robotic surgery. Sending Cobra down a patient’s throat is minimally invasive as it avoids splitting the jaw and with more accurate treatment it helps improve patient outcomes,” says Olaleye.
“The future potential for Cobra is limitless. Not only can various devices be bolted onto the ‘head’, such as sensors for next-generation AI diagnostics, but it can also be used in other areas of the body, including the chest and bowel.”

8
Wearable ECG monitor for real-time heart health

Patients suffering with heart conditions such as an abnormal heartbeat, known as arrhythmia, often need close monitoring by healthcare professionals. Current options include restrictive and intrusive ECG monitors to detect anything unusual with the heart’s rhythm and electrical activity.
To offer patients comfort and peace of mind, a team at PA Consulting has developed an ECG monitoring system that is simply integrated into the patient’s T-shirt. This discreet device continually monitors the patient’s heart for weeks or months.
Sara Urasini, wearables expert at PA Consulting, says: “Viscero isn’t just about technology; it’s about improving healthcare experiences for doctors and patients. It does away with bulky sensors and invasive set-ups by cleverly incorporating dry electrodes into the garment construction for continuous heart monitoring. It allows its wearer to have the freedom of their everyday life, whilst effortlessly capturing a medical-grade signal that can prevent or monitor heart-rhythm irregularities such as arrhythmia.”
Together with recorded ECG signals, the device also includes an accelerometer and gyroscope to provide healthcare professionals with a fuller picture of the circumstances surrounding an arrhythmia event.
This diagnostic data is sent to an AI-enabled dashboard where doctors can easily identify arrhythmia events without having to scroll through ECG recordings. Patients can view results and correspond with their doctors via a mobile app.
9
Soft robotic implants for drug delivery
Implantable devices offer exciting prospects for tailored drug delivery, such as the correct dosage of insulin to diabetic patients. However, the challenge with these devices, especially for long-term use, is the scar tissue the body naturally creates in response to them.
“If anything foreign enters our bodies, like bacteria, the immune system will immediately attempt to break it down. If it cannot be broken down, like if it’s an implantable plastic device, the immune system will instead wrap it in a connective type of fibrous tissue or scar tissue. This often prevents drug release as the tissue can be dense and impermeable,” says Dr Rachel Beatty at the University of Galway.
Beatty is part of a team from the University of Galway and the Massachusetts Institute of Technology that is researching implantable devices. These devices use AI to monitor the formation of scar tissue, which can differ from patient to patient. Then soft robotics is deployed to enable the device to make regular movements, such as inflating and deflating, to help prevent scar tissue from forming.
“So far we’ve successfully shown through computational models how the implant can finely control drug release. We still have more research to do but this approach could generate revolutionary changes in implantable drug delivery for not only diabetes but a range of chronic diseases,” says Beatty.
10
Device continually monitors IV therapy

Most hospital patients are fitted with an intravenous (IV) device, a thin plastic tube inserted directly into a vein for the administration of medication, fluids and blood products.
While IV insertion is a common hospital procedure, IV leakages, known as extravasation, do often occur. This can cause patient harm, drug delivery errors, scarring, nerve damage and possibly even death.
For more than 10 years, Virginia-based ivWatch has been developing a device that is applied to the skin near the site of the IV device to continuously monitor for any signs of infiltration or extravasation events.
ivWatch’s chief operating officer Jaclyn Lautz says: “The lurking dangers of IV therapy can be quite scary, but now, with the addition of continuous patient monitoring, nursing staff and patients alike can have peace of mind.”
ivWatch includes a patient monitor and a smart touch sensor paired with a predictive algorithm. Light signals are emitted from the sensor’s LEDs and into the tissue near the IV site. Reflected light signals are received by the photodiode in the sensor and transmitted for analysis by ivWatch’s proprietary algorithm.
By detecting specific changes between the emitted and reflected light signals, it determines whether conditions indicate that an infiltration or extravasation event may have occurred.
“ivWatch is a necessary aid for any busy nursing staff because it monitors the IV site, alerts clinicians in real time and acts as the first line of defence against IV injury due to its high degree of sensitivity and accuracy,” says Lautz.